The Accidental Drug Advocate - Latest What Your GP Doesn't Tell You Podcast
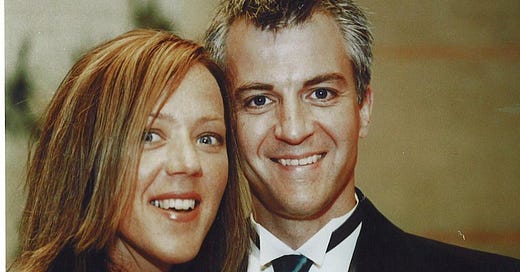
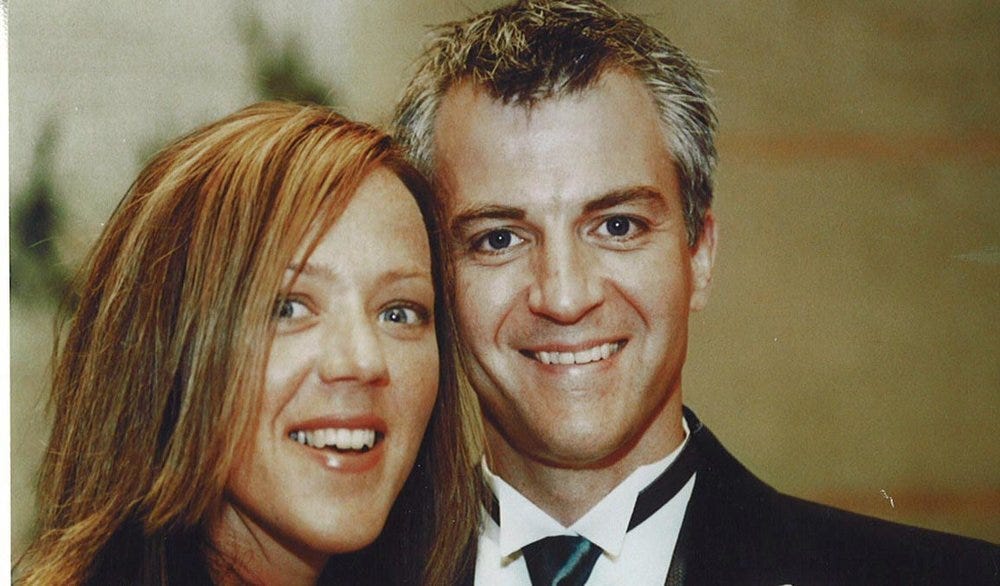
Kim Witczak explains how her husband Woody's suicide has driven her 20 year campaign for safer drugs
The latest episode of the What Your GP Doesn’t Tell You Podcast - The Accidental Drug Advocate is now available on Apple, Spotify and other podcast platforms. And you can sign up to the podcast mailing list at What Your GP Doesn't Tell You, where you can also find out more about the pod. The podcast will now be taking a short break and will back on Tuesday 14th November.
This week, I am talking to Kim Witczak whose life changed tragically twenty years ago. Nothing would ever be the same again. Her husband, Woody, had been struggling with insomnia, and so in 2003, his GP gave him a prescription for a drug called Zoloft (in other countries the medication has different names including: Contulen & Lustral. The drug’s generic name is sertraline). Woody had no history of depression or mental illness.
Puzzlingly, he began experiencing symptoms that he had never felt before. Neither he, Kim or his doctor imagined this could be in any way connected to the medication he was taking:
Several weeks later, Kim had to go on a work trip to Detroit and she became increasingly worried one day when Woody wasn’t answering his phone.
Following Woody’s suicide, Kim decided to sue the manufacturer of Zoloft, Pfizer, for his wrongful death.
And as Kim and Woody’s relatives began to investigate further, they discovered that the FDA had held hearings, 12 years earlier in 1991, to explore if there was any evidence of a link between the SSRI anti-depressant drug Prozac (generic name fluoxetine) and violent and suicidal reactions. The FDA concluded: ”there was no credible evidence of a causal link between the use of antidepressant drugs, including Prozac, and suicidality or violent behaviour”.
At the time of the hearing, the FDA had received over 14,000 reports of side effects from Prozac, but while many families felt the drug was responsible for their family member’s death or violent actions, a number of experts gave evidence suggesting that any violence or suicidality was the result of illness - not the medication that they were taking.
But the debate continued, and Kim argues that documents that came out of her lawsuit provided evidence that the drugs could induce a greater risk of suicide, something denied by the manufacturer:
As Kim says, today the US drug label warning only extends up to patients 24 years old or younger, not adults of Woody’s age. But the UK and European warning is worded slightly differently, which while emphasising a greater risk for young adults, does appear to include all age groups:
“If you are depressed and/or have anxiety disorders you can sometimes have thoughts of harming or killing yourself. These may be increased when first starting antidepressants, since these medicines all take time to work, usually about two weeks but sometimes longer.
You may be more likely to think like this:
• If you have previously had thoughts about killing or harming yourself.
• If you are a young adult. Information from clinical trials has shown an increased risk of suicidal behaviour in adults aged less than 25 years with psychiatric conditions who were treated with an antidepressant”.
In the end, Kim’s lawsuit with Pfizer was settled out of court. The process took just over two years and the exact terms of the settlement cannot be disclosed. The company did not admit liability.
One particular side effect of the SSRI antidepressants, which Kim says far more patients and GPs need to be conscious of, is a condition called akathisia, which is something that Woody experienced while on the drug. It’s described as a sort of inner restlessness.
Today, Kim sits as the consumer representative on the Food and Drug Administration (FDA) Psychopharmacologic Advisory Board Committee, which recommends whether a drug should be approved or not. Its advice is not binding but the FDA usually follows it.
Kim says from her experience on the committee, she believes that safety is not given a high enough priority, and that especially with the fast tracking of certain drugs, some medications are approved too quickly. And we discussed in the podcast how this can be a difficult balance, because the flipside is patients who are seriously ill may be desperate for a new drug, and want the trial process speeded up as quickly as possible.
The standard requirement for a drug to be approved is for it to have two randomised double-blind clinical trial results that show it has a statistically significant benefit over a placebo.
However, as Kim explains in the podcast, drugs fulfilling an unmet need may only require one clinically positive randomised double-blind trial and she discusses one case where only 95 people in the clinical trial had taken the active drug, before the medication was approved. And she reveals her concerns about how the process has worked in the past, which has led to decisions she firmly disagrees with. She argues it’s essential that the system changes for both the benefit of patients and doctors.
Kim Witzcak is a co-founder of Woodymatters, a non-profit dedicated to advocating for a stronger FDA and drug safety system. She is on the board of directors of National Physicians Alliance and MISSD. (MISSD stands for Medication Induced Suicide Prevention in Memory of Stewart Dolin). And Kim is also an active member of the DC-based Patient, Consumer, and Public Health Coalition, that aims to ensure that the voice of non-conflicted patients and consumers is represented in healthcare and FDA related legislative issues.
You can find out more about the podcast at What Your GP Doesn't Tell You and follow me on Twitter @lizctucker.
Putting together a podcast like this requires a large amount of work and resources, so if in the coming weeks you feel able to support the podcast, I’d be very grateful. You can do so at patreon.com/whatyourgpdoesnttellyou or on PayPal at What Your GP Doesn't Tell You.